IVF was the first procedure used to fertilize eggs outside a woman’s body. In 1978, the first “test tube baby,” was conceived through IVF. Most assisted reproductive technologies (ART) are derived from the IVF procedure.
IVF was the first procedure used to fertilize eggs outside a woman’s body. In 1978, the first “test tube baby,” was conceived through IVF. Most assisted reproductive technologies (ART) are derived from the IVF procedure.
Follicle stimulation and monitoring
The same hormones that stimulate one egg to be produced each cycle are given to the woman in higher doses to produce multiple eggs in the ovary. These medications are given at home by the woman herself, much the same way a diabetic gives herself insulin injections.
During this stimulation process which takes about 10 days, the woman is seen in the office 5-6 times for vaginal ultrasound assessment of follicle (egg) growth and blood estrogen determination. These visits tell the doctor how many eggs are being stimulated and when they are ready to be retrieved. A minimum number of follicles must develop to make the retrieval worthwhile. Cancellation or postponement of the cycle may occur if there are too few or too many follicles noted on ultrasound.
Oocyte (Egg) Retrieval
Egg retrieval is performed while the woman is asleep under sedation provided by Nurse Anesthetists. The doctor inserts a needle through the vagina into the ovaries and into each follicle using ultrasound guidance. The follicle fluid containing the egg from the follicle is aspirated into test tubes and given to the embryologist for egg identification. Each egg is then placed in an incubator where it will be placed with sperm a few hours after the retrieval. The number of eggs retrieved can range from 0 (rarely) to 30 (rarely) depending on the age of the woman and her ovarian sensitivity.
The egg retrieval takes approximately 20 minutes, and the woman then recovers in the recovery room until she is ready to return home for a day of rest on the day of egg retrieval.
Please Note: Due to potential complications with anesthesia, the Center for Reproductive Medicine does not offer IVF to patients with a BMI that is greater than 37.
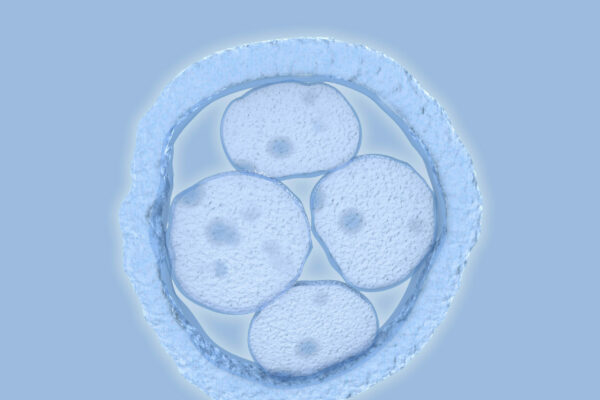
Fertilization and Incubation
The eggs and sperm are mixed in the laboratory to allow fertilization. In over half of IVF cycles, the embryologist injects a single sperm directly into an egg – this technique is called Intracytoplasmic Sperm Injection (ICSI) – and is used in cases of low sperm counts or when our pre IVF sperm testing suggests a high chance of poor spontaneous fertilization. On average, 70 percent of mature eggs will fertilize. The embryos will be placed in an incubator where their growth will be monitored for 3-5 days. Most embryos are transferred on day 5 after retrieval at the “blastocyst” stage. Some embryos are transferred on day 3 at the “cleavage” stage, depending on the number of embryos and their growth pattern.
Embryo Transfer Procedure
Our goal is to transfer the embryo/s that will optimize your chance to conceive but minimize the chance for multiple pregnancy with its associated risks for mother and baby. For women under age 35 with good quality embryos and embryos to freeze the combined pregnancy rate with a single fresh embryo transfer followed if necessary by a single frozen embryo transfer is just as good as a fresh two-embryo transfer but without the risks and expense associated with twins.
The embryos are transferred to the uterus through a soft catheter passed through the cervix. The procedure does not require anesthesia, and resembles a PAP smear, except that we ask you to have a full bladder so that an abdominal ultrasound can guide the physician in the optimal placement of the embryos. After a short stay in the clinic, the woman is driven home for one day of “couch rest” to allow the embryos to implant in the uterus.
The physician will prescribe Progesterone administered vaginally twice daily, and estrogen patches changed twice weekly until the pregnancy test is obtained two weeks after the egg retrieval. If the cycle was successful Progesterone will usually continue for at least another month. (See our Success Rates).
Cryopreservation
If there are more embryos available after the transfer that have reached the blastocyst stage, the couple may freeze these embryos for future use. If the fresh transfer was unsuccessful the frozen embryo/s may be thawed and transferred within two months. If the fresh cycle was successful and the couple wishes another pregnancy the embryos can be thawed and transferred years from the initial egg retrieval.
Transfer of cryopreserved embryos
This procedure uses embryos that were saved from a previous IVF cycle and frozen. The embryos are thawed and transferred into the uterus after a specialized protocol which prepares the lining of the uterus for implantation. It is simpler and less expensive than a “fresh” IVF cycle since no stimulation and egg retrieval are required. (See our Success Rates).
TESE
In cases where there is no sperm in the ejaculate, there is sometimes sperm in the testicle. In these situations, a male infertility specialist can remove testicular tissue for our laboratory to examine microscopically. If viable sperm are found they can be used for IVF with ICSI. For more information see Testicular Sperm Extraction (TESE).
Preimplantation Genetic Testing-Mutation (PGT-M)
Preimplantation Genetic Testing-Mutation (PGT-M) is genetic testing of embryos conceived with IVF to avoid transmission of familial single gene dominant and recessive diseases like Huntington’s disease and Cystic Fibrosis or Muscular Dystrophy, or structural chromosome defects like translocations or inversions. It may also be used to lower the age-associated increased occurrence of miscarriages or chromosomal trisomies like Down syndrome. There are also some data to suggest it may increase the delivery rate in couples with recurrent pregnancy loss.
PGT-M is still considered investigational, though its use is increasing.
In PGT-M, the embryologist removes cells from each embryo created in the IVF cycle. The cells are tested for abnormal genes or chromosomes. Only the embryos that have normal cells are transferred into the woman. Although PGT-M is 99% accurate, misdiagnoses have been made, so couples often confirm the PGT-M diagnosis with chorionic villus sampling (CVS) or amniocentesis later in the pregnancy. Not all genetic diseases can be detected, nor can all chromosomes be evaluated.
Gestational Surrogacy
If a woman does not have a functional uterus but has normal ovaries, eggs can be retrieved from the woman with normal ovaries, fertilized, and the resulting embryos transferred into a “gestational carrier” or a woman with a normal uterus who would carry the pregnancy. Following the pregnancy and delivery, the child would be returned to the woman/couple. Legal counsel from attorneys who specialize in family law is recommended in these cases.